For MF patients or their caregivers; I am not a doctor. Please do your own research if this information does not line up with your understanding.
The new dates are booked–December 6th R gets admitted to the University of Washington Medical Center for chemo and December 12th he’ll get the donor stem cells (transplant). In his high-risk condition, he’d have months to a year to live without the transplant. So, HURRAH! HOORAY! YAY! GRATEFUL! RELIEVED!
Someone asked today how the donor cells get infused. Good question.
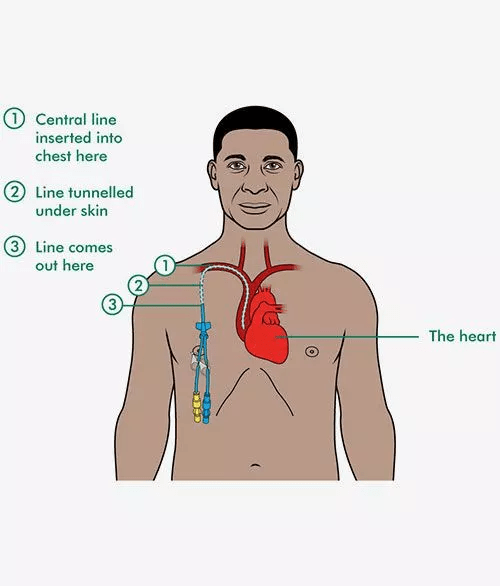
R had a type of port put in at the hospital. A “Hickman line” (see illustration) is a long, thin, soft, silicone tube (catheter) that provides long-term access to the large vein in the heart. It’s inserted into the chest wall under local anesthetic and is used for chemotherapy, intravenous (IV) therapies, medication administration, IV nutrition, blood transfusions of which he’ll need many over the coming months, and to draw blood for labs without needing repeated needle sticks. The line is tunneled under the skin and exits through his chest.
From the web:
Allogeneic Bone Marrow Donor Process (meaning bone marrow from a matched donor, as opposed to specially treated blood that is extracted from and goes back into the same person/patient).
DONOR PROCESS:
- Preparation: The donor gets daily injections to speed up stem cell production.
- The Donation Procedure (Marrow Harvest):
- The procedure is performed in an operating room, usually under general anesthesia.
- A sterile, hollow needle is inserted through the skin into the hip bone.
- Liquid bone marrow is withdrawn, typically about 1 to 2 pints (about 10% of the donor’s total marrow).
- The procedure usually takes 1 to 2 hours.
- Post-Donation and Recovery:
- The donor is moved to a recovery room and leaves the hospital the same day or next morning.
- The donor may experience soreness, bruising, and aching in the lower back/hips, and feel tired for a few days to a few weeks.
- Over-the-counter pain medication manages discomfort, and the body naturally replaces the donated marrow in 4 to 6 weeks.
- Donors typically return to work or school within 2 to 7 days.
- Stem cells are transported/flown to the patient (in this case from Germany to Washington State) within 12 hours.
PATIENT/RECIPIENT PROCESS
Meanwhile, for the patient receiving the transplant:
- Conditioning: The patient undergoes *two-step chemotherapy (5 days hospital inpatient) to destroy most of the cancerous cells and make room for the new ones. *This is the case for R’s transplant and may be different in other cases.
- Infusion: The donor cells are given to the patient through the Hickman port. (Not painful.)
- Engraftment: The new stem cells travel to the patient’s bone marrow and begin to produce healthy blood cells, a process called “engraftment,” which typically takes 2 to 4 weeks and up to 3 months.
- Monitoring and Recovery: The patient requires a hospital stay of several weeks to months and is closely monitored for infections and complications, such as graft-versus-host disease (GVHD). Full immune system recovery can take much longer, sometimes up to a year or more.
- The journey after R comes home will be dangerous and scary. Keeping him free of infection will be a life or death endeavor, plus watching for signs of GI tract and lung problems, medication complications, low blood counts, weight loss, skin issues/rash/pain, fever, bone pain and more.
YOUR PRAYERS, BEST WISHES AND EMOTIONAL PRESENCE GIVE US STRENGTH AND MAKE US HOPEFUL.
R will not be able to receive flowers or plants in the hospital or at home because of spores, mold, etc. You can always send him a card which I will give to him. Let me know if you need our address. Thanks to our daughter for staying at our house while I’m mostly away.
SAVE A LIFE
If you are under 40 years old, you can register to be a stem cell donor at the National Bone Marrow Registry.
Anyone, age 16+ can donate platelets by appointment at any American Red Cross location or Bloodworks Northwest. It takes 1-2 hours and is similar to a regular blood donation.
- Many myelofibrosis (MF) patients often need 2-4X more platelets than other transplant patients because their disease uses up or destroys platelets faster, and the bone marrow cannot keep up.


Leave a comment